This "Forschungsgruppe" is a highly interdisciplinary research team from the Institute of Cancer Research of the Medical University of Vienna together with the Institute of Analytical and Inorganic Chemistry from the University of Vienna.

Due to improved diagnosis and therapy, survival of cancer even at an advanced stage of the disease is increasing. Noteworthy, besides the novel forms of systemic cancer therapy, including targeted compounds and immunotherapy, also classical chemotherapy e.g. with platinum drugs is still an important and effective therapeutic strategy.
Supported by the novel high-end technologies and the massive increase of know-how concerning the nature of cancer, also chemotherapy gets more precise and effective. Additionally, it becomes increasingly obvious that also for metal-based chemotherapy precise targeting mechanisms exist. Thus, not only the direct cytotoxic activity against the tumor cells, but also e.g. immune effects are important for a successful therapy response. However, still positive outcomes are not achieved in every patient and side effects, although nowadays much better manageable, are still one of the key limiting factors of cancer cure.
Consequently, our cooperative project network aims to improve the quality of platinum-based systemic cancer therapy in several directions:
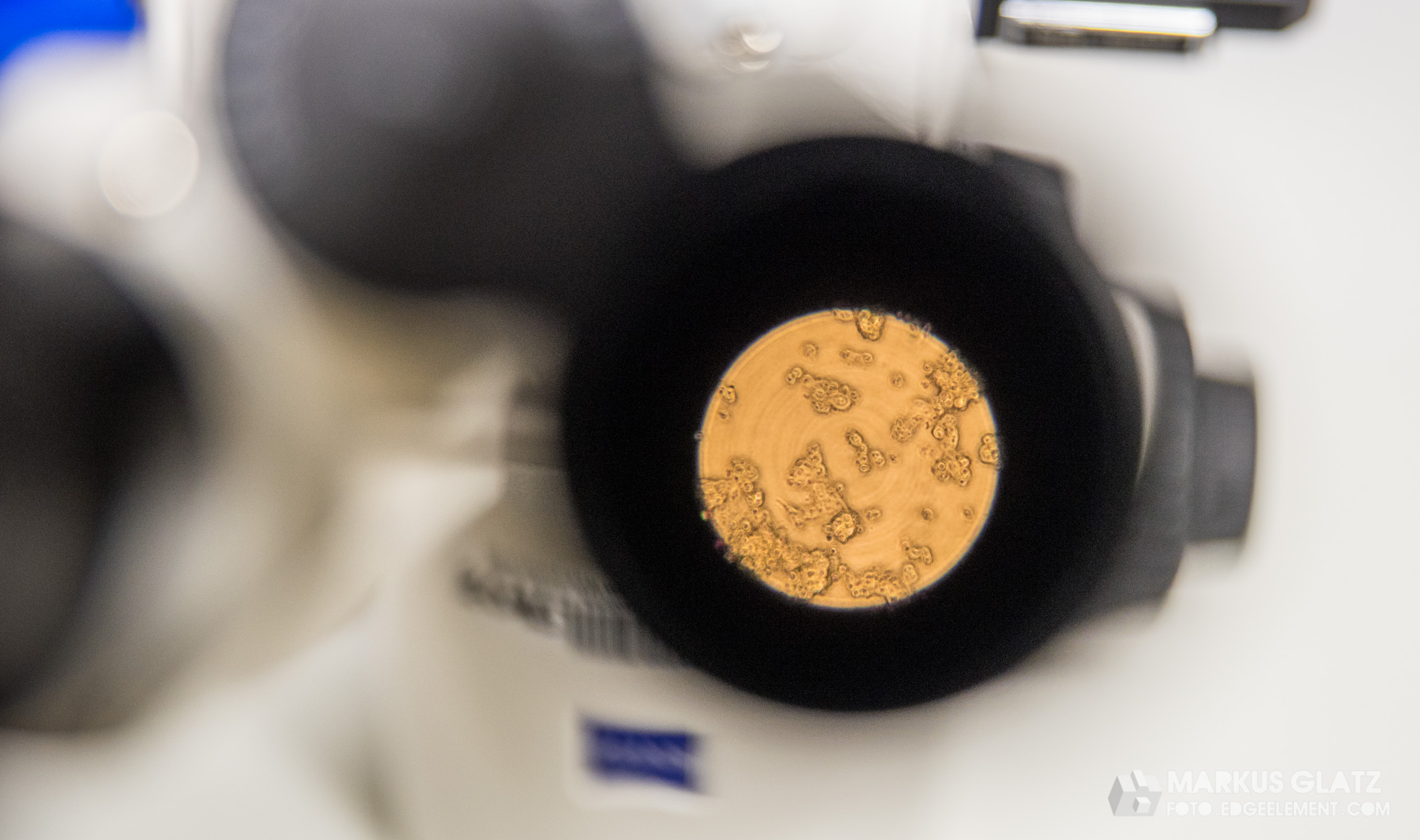
- We want to analyze the fate and the impact of clinically used and experimental platinum compounds down to the single cell level of the cancer tissue comprising in addition to the tumor cells also blood vessels, stroma and immune components. For these single cell analyses, high-end analytical techniques are available in our consortium and will be optimized in course of this project.
- Concerning novel remedies, the focus will lie on manipulating not only the cancer cells but also the direct environment of the tumor (as the surrounding tissues like stromal cells, immune cells etc. is often “abused” and altered by the tumor to support its needs). This should allow improved tumor control and reduced therapy failure by resistance development often caused by alterations in both tumor cells and microenvironment. Moreover, besides enhancing the anticancer effect, we aim to reduce the side effects by activating the cytotoxic activity of the metal drugs specifically inside the malignant tissue.
From old to new: Platinum drugs heading for the future
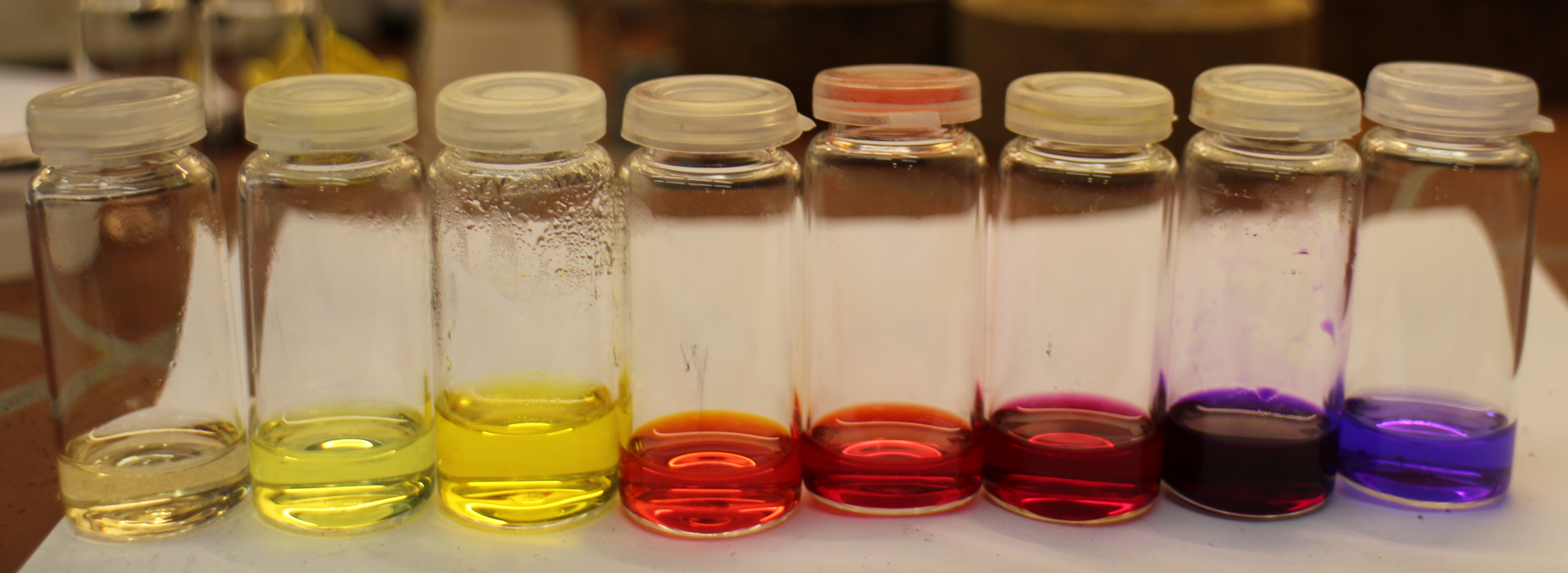
Strategically, already successfully used platinum drugs will be altered (oxidized) in a way that leads to reduced toxicity in the health tissue, and the ability to synthetically attach up to two additional chemical moieties (including other drugs supporting the platinum compound or delivery structures allowing to enhance accumulation in the malignant tissue). Consequently, only in the chemically altered environment of the malignant tissue, these per se non-toxic compounds (prodrugs) should be activated and release their cell killing activities.
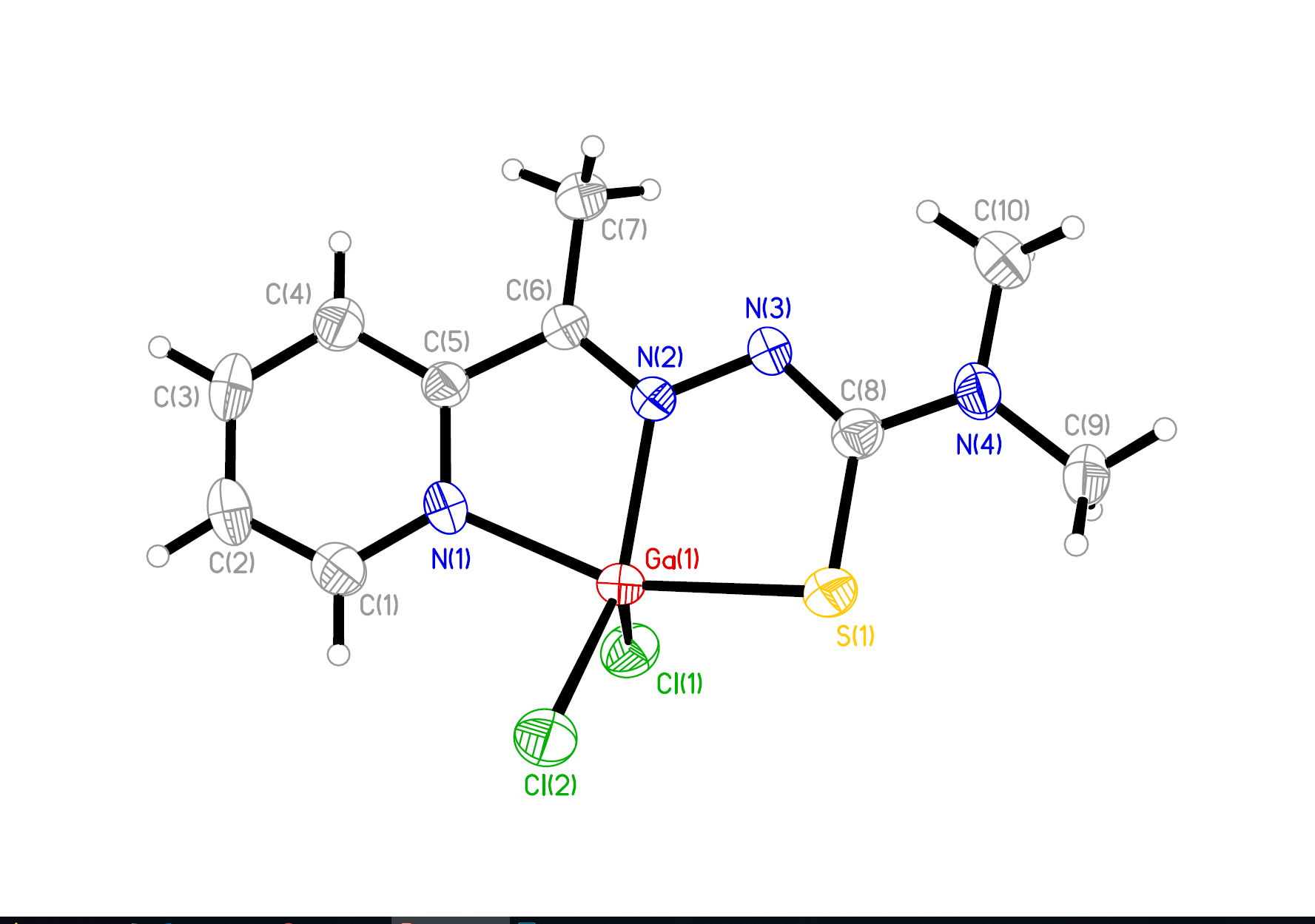
In order to fulfill such a challenging task successfully, multidisciplinary cooperations like in this consortium are essential, including synthetic chemists (generating the novel remedies), analytical chemists (able to precisely determine the fate of the remedies on their impact on the organism), as well as cancer biologists and toxicologists (to test the compounds´ activities and adverse effects using diverse models systems). In detail, our strategies comprise the development of anticancer platinum prodrugs specifically targeted to the tumor (via binding to the main blood protein albumin which is efficiently degraded by the tumor but much less by health cells) and releasing in the malignant tissue besides the cytotoxic chemotherapy (cisplatin, oxaliplatin) also immune-stimulating agents. Finally, therapy response/failure will be traced back to the contribution of metabolic factors and the tumor architecture down to the single cell level with a specific focus on the role of fibroblasts and immune cells.
Research Group
Publications
- Mathuber, M. et al. Development of a cobalt(III)-based ponatinib prodrug system. Inorg. Chem. Front. 2021, 8, 2468–2485. doi.org/10.1039/D1QI00211B
- Schueffl, H. et al. Albumin-targeting of an oxaliplatin-releasing platinum(iv) prodrug results in pronounced anticancer activity due to endocytotic drug uptake in vivo. Chem Sci. 2021 Aug 26;12(38):12587-12599. doi: 10.1039/d1sc03311e.
- Fronik, P. et al. A platinum(IV) prodrug strategy to overcome glutathione-based oxaliplatin resistance. Comm. Chem. 2022, 5, 46 . doi.org/10.1038/s42004-022-00661-z
- Hohenwallner K et al. JACS Au. 2022 Oct 25;2(11):2466-2480. doi: 10.1021/jacsau.2c00230. eCollection 2022 Nov 28.
- Mendrina, T. et al. Influence of the Fatty Acid Metabolism on the Mode of Action of a Cisplatin(IV) Complex with Phenylbutyrate as Axial Ligands. Pharmaceutics 2023, 15, 677 . doi: 10.3390/pharmaceutics15020677.
- Kastner, A et al. Tumor-targeted dual-action NSAID-platinum(IV) anticancer prodrugs. Inorg. Chem. Frontiers 2023, 10, 4126-1438. doi.org/10.1039/D3QI00968H.
- Schaier, M. et al. Human Serum Albumin as a Copper Source for Anticancer Thiosemicarbazones. Metallomics 2023, 15, mfad046
- Caban, M. et al. A novel EGFR inhibitor acts as potent tool for hypoxia-activated prodrug systems and exerts strong synergistic activity with VEGFR inhibition in vitro and in vivo. Cancer Lett. 2023, 565, 216237. doi: 10.1016/j.canlet.2023.216237.
- Kastner et. Et al. Insertion of (bioactive) equatorial ligands into platinum(IV) complexes. Angew. Chem. 2023, 62, e202311468. https://doi.org/10.1002/anie.202311468.
- Van Acker, T. et al. Inductively coupled plasma mass spectrometry (2023) Nature Reviews Methods Primers, 3 (1), art. no. 52, DOI: 10.1038/s43586-023-00235-w
- Baier, D. et al. The Lipid Metabolism as Target and Modulator of BOLD-100 Anticancer Activity: Crosstalk with Histone Acetylation (2023) Advanced Science, 10 (32), art. no. 2301939. DOI: 10.1002/advs.202301939
- Metarapi, D. et al. Semiquantitative Analysis for High-Speed Mapping Applications of Biological Samples Using LA-ICP-TOFMS (2023) Analytical Chemistry, 95 (19), pp. 7804-7812. DOI: 10.1021/acs.analchem.3c01439
- Babu, T. et al. Oral Anticancer Heterobimetallic PtIV−AuI Complexes Show High In Vivo Activity and Low Toxicity (2023) Angewandte Chemie - International Edition, 62 (10), art. no. e202217233 DOI: 10.1002/anie.202217233
- Schaier, M. et al. Multiparametric Tissue Characterization Utilizing the Cellular Metallome and Immuno-Mass Spectrometry Imaging (2023) JACS Au, 3 (2), pp. 419-428. DOI: 10.1021/jacsau.2c00571
- Kastner, A. et al. Stepwise Optimization of Tumor-Targeted Dual-Action Platinum(IV)-Gemcitabine Prodrugs. Inorg. Chem. Frontiers 2024, 11, 534-548 (IF = 7.0), DOI: 10.1039/D3QI02032K.